Contracting with Healthplans and Managed Care Organizations
As a result of healthcare reforms enacted by Congress, Healthplans, and managed care organizations across the country are being challenged to improve access, improve outcomes and reduce health care costs. Healthplans are challenged by the need to create alternative payment methods that can lead to value-based contracts. Such contracts may include options such as pay-for-performance, risk-sharing and/or value-based reimbursement.
Using the tools offered by Private Practice Cloud (PPC), psychotherapists in solo or group practices or operating as Independent Practice Organizations can negotiate contracts with Healthplans and offer viable value-based reimbursement or payment strategies that:
Link value directly to performance.
Link performance to reimbursement.
Link reimbursements to coordination of care with medical professionals.
The purpose of PPC dashboards is to quickly quantify, analyze, and correlate the cost of care against meaningful clinical outcomes across different providers. These interactive dashboards can empower patients, physicians, therapists and Healthplans to proactively explore and support continuous improvement strategies based upon variances in both outcomes and costs. The designers of these dashboards partnered with clinicians to build a visual analytics platform driving value-based patient care, quality, and cost efficiencies.
Service examples that can be linked to quality & value
Urgent & timely Routine Services
We have technology that gives patients or approved professional referrers the ability to schedule tentative appointments and allow clients to manage routine appointments with providers.
Measuring timely access to services has value.
Patient Reported Outcome Measures
Category 1 healthcare services are fee-for-service methods that do not demonstrate a measurable value and benefit to patients.
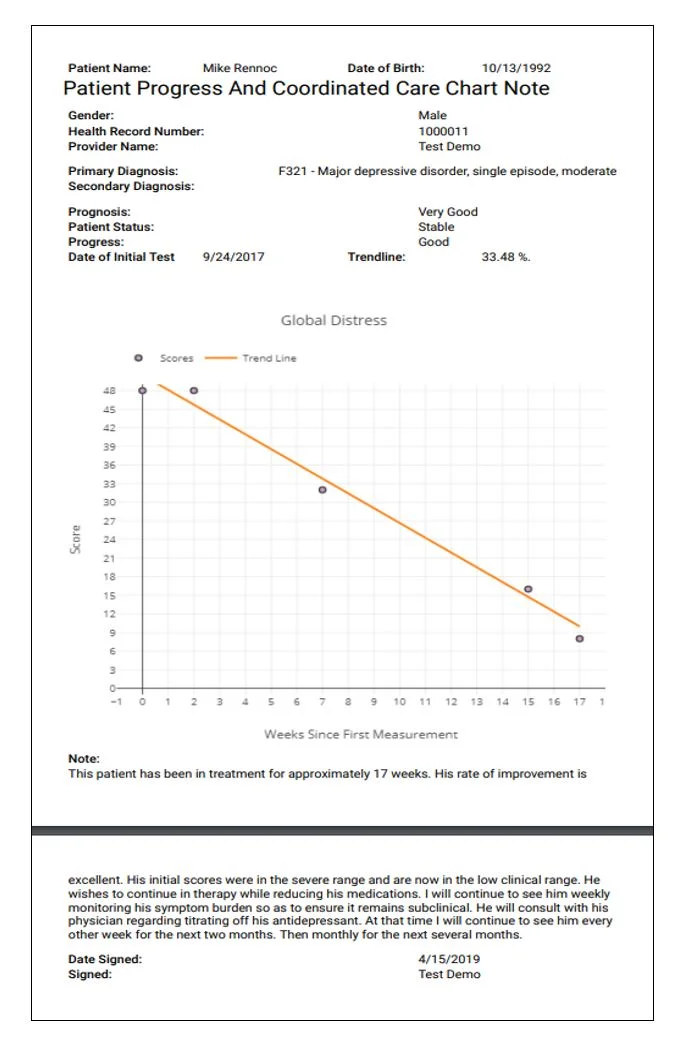
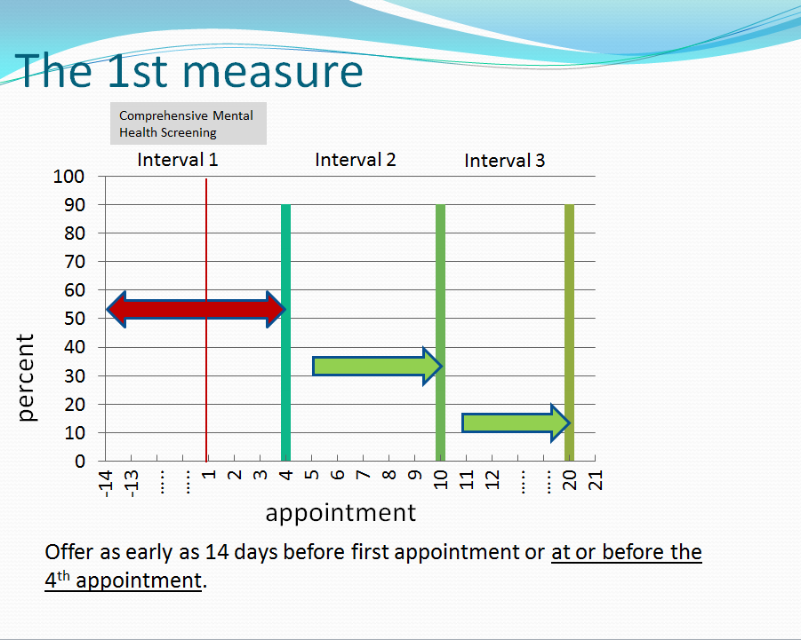
Patient reported outcome measures (PROMs) are proven strategies to demonstrate and improve outcomes in medical and behavioral health. The use of PROMs in patient-centered and coordinated care is recognized by both the federal government and the healthcare industry as a means to link value to services provided.
The use of PROMs moves payment to Category 2 where services are linked to measurable value.
Measurement Strategies that are helpful
Linking patient reported outcomes measures to value is simple concept that requires small changes in a providers work flow and is made easier using technology that can gather data, securely save that data, and display the data as graphic information that can be privately and effectively shared by psychotherapists with patients and their medical caregivers.
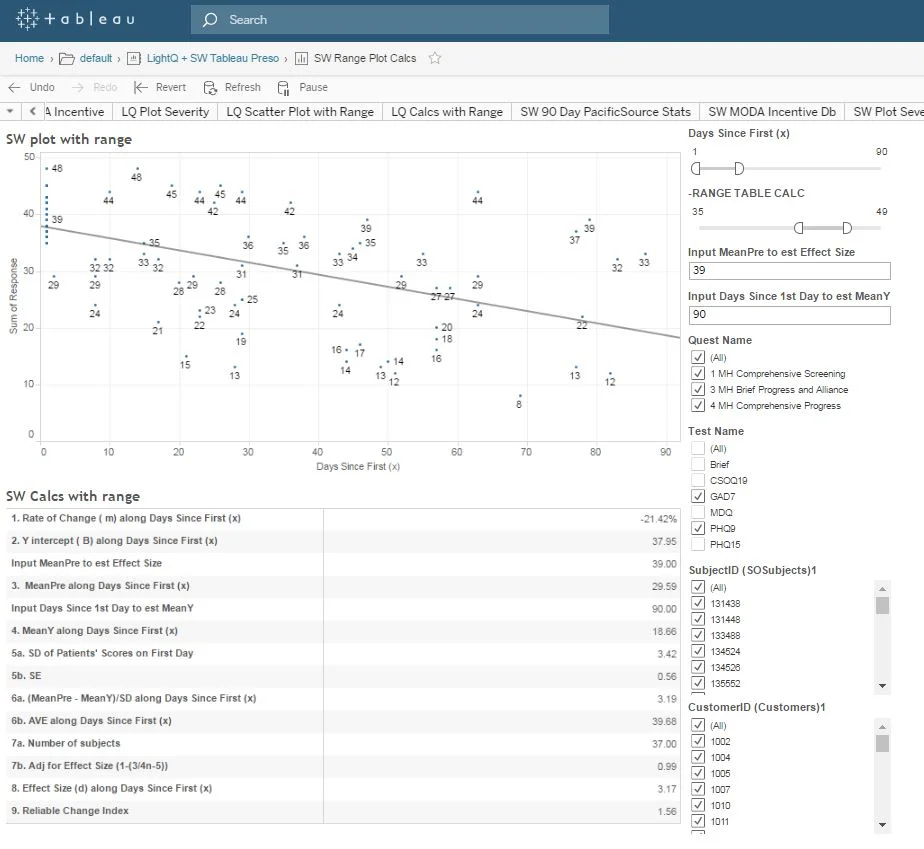
Services Linked to MEASURABLE Value
Sharing dis-identified outcomes information with Healthplans allows the Healthplan to demonstrate the value of their coverage to their providers and customers. The purpose of this dashboard is to quickly quantify, analyze, and correlate the cost of care against meaningful clinical outcomes across different providers. Interactive dashboards can empower patients, providers and Healthplans to proactively explore and support continuous improvement around variances in both outcomes and costs.
Standardized Cost-Benefit Comparisons
Standardized Visual Cost-Benefit Analysis
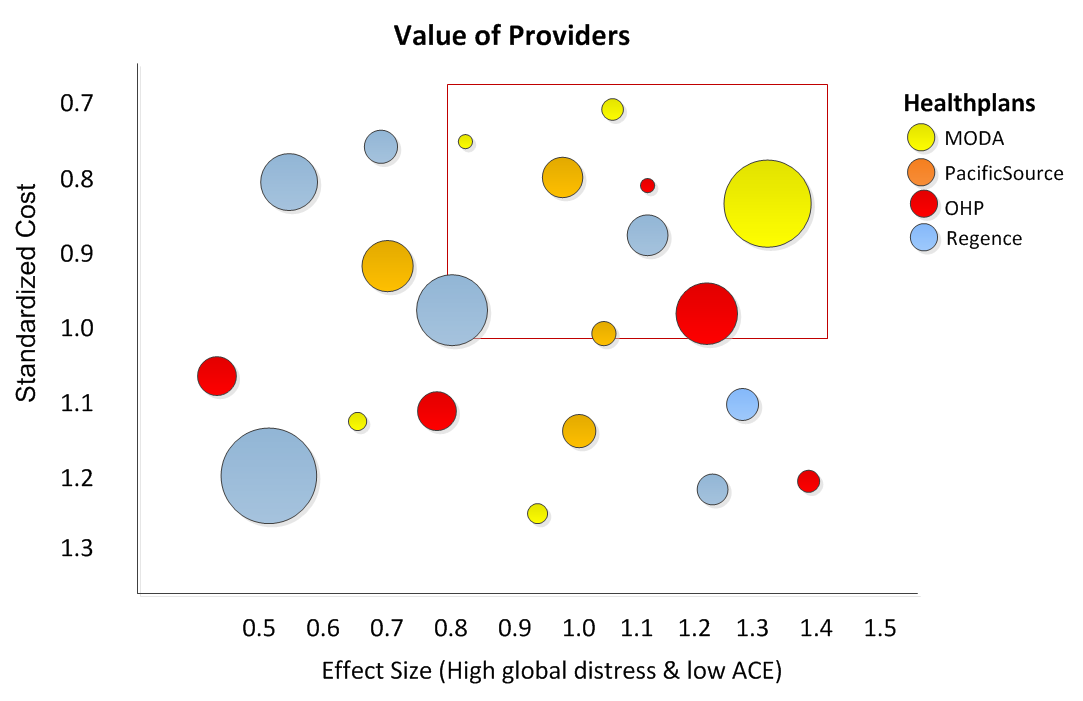
A standardized cost is numeric calculation remove the variance variance among all CPT codes charges and compares that to providers ariance. for all providers can compares and normalized. In the figure title “Value of Providers” each circle represents a provider. The size of the circle represent the number of patients in an episode of care. Each color represents a specific Healthplan. The area delineated in the red box identifies those providers who have lower relative cost and better outcomes. The larger the effect size number the greater the effect (providers to the right are better). The lower the standardized cost number the less expensive, (Up is good).
Standardization of reimbursements means adjusting the amount of reimbursement among providers with the same CPT codes, but different reimbursements rates, to a common scale. When provider outcomes are standardized, the standardardized cost of a provider’s services can be compared to the effect size of their outcomes. The effect size is the standardized outcome of providers treating similar patients. This contrast can provide a useful visual representation of value. The providers in the red outlined box have a significantly better outcome and a significantly lower cost. The primary advantages to using a standard scaling is that it can be used for adjusting reimbursements based on value, controlling costs, and to support decision-making purposes.